By Diana I. Ortiz, Zachary P. Fryda, and John Bower
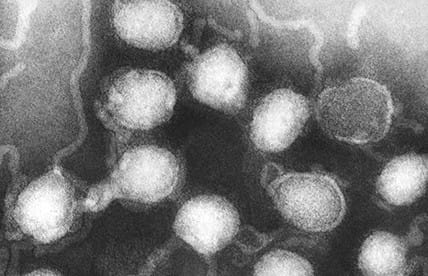
Arboviruses are arthropod-borne pathogens transmitted through the bites of infected arthropods, such as mosquitoes and ticks. Most arboviral infections are asymptomatic or mild, but neuroinvasive disease can occur most often presenting as encephalitis or meningoencephalitis. La Crosse encephalitis virus (LACV), a national notifiable disease, is the most common cause of pediatric arboviral infections in the United States, with a high prevalence in eastern Ohio, near the Pennsylvania border.
Historically, most cases of LACV infections have occurred in the upper Midwestern US, but recently, more cases have been recognized in the Appalachian region. Cases occur primarily from late spring through early fall, mostly in rural and suburban locations. People contract LACV from bites of its main vector, Aedes triseriatus, the eastern tree hole mosquito. Amplifying hosts include small mammals, such as chipmunks and squirrels, which can develop levels of viremia sufficient to transmit LACV to mosquitoes. Two other mosquito species, Ae. albopictus and Ae. japonicus, have also been found naturally infected with LACV. These mosquito species are aggressive daytime biters, readily feed on humans, and breed in natural and human-made containers, including tree holes, discarded tires, and other items that may retain water for at least seven days. These ecological characteristics enhance the vector’s potential for human contact, which may increase the chance for LACV transmission.
Although serological evidence suggests that most LACV infections are asymptomatic or subclinical, those who become ill may develop severe neuroinvasive disease. Disease onset ranges from 5 to 15 days post exposure. Signs and symptoms of encephalitis can be confused with other infections, such as herpes simplex and enteroviral or with bacterial meningitis. In the US, an average of 65 LACV neuroinvasive disease cases are reported annually. Encephalitis initially presents as a nonspecific summertime illness with fever, headache, nausea, vomiting, and lethargy. Although, deaths are rare (<1% of clinical cases), neuroinvasive disease occurs most commonly in children under the age of 16, which is characterized by seizures, coma, paralysis, and a variety of neurological sequelae, like recurrent seizures, hemiparesis, or cognitive and neurobehavioral abnormalities. Long-term sequelae represent a substantial health and economic burden, with an estimated cost of over 3 million dollars per patient. Cases among siblings and neighborhood children have occurred over a period of years, which may indicate foci of more intense virus-vector activity.
Preliminary diagnosis is often based on the patient’s clinical features, travel history, outdoor activities, and geographic location of infection. The virus is difficult to identify from clinical samples using culture or nucleic acid testing. As a result, serologic testing remains the primary method for diagnosing LACV infection. Combined with a consistent clinical presentation in an endemic area, a rapid and accurate diagnosis of acute neuroinvasive disease is made by the detection of LACV-specific IgM antibody in serum or cerebrospinal fluid. LACV IgM titers, however, may be negative within the first 10 days of illness. In these cases, diagnosis is made by showing a four-fold increase in the LACV IgG titer between acute and convalescent patient samples. Although, no vaccine against LACV infection or specific antiviral treatment is available, supportive treatment, including seizure control, is provided to patients. The most effective way to prevent infections from LACV is through avoidance of mosquito bites and the elimination of mosquito breeding sites by cleaning and/or removing containers that may hold water for at least seven days.
Since 2000, Pennsylvania has reported only one case of LACV. Due to the close geographical proximity of cases reported in nearby Ohio border counties in recent years and the ecological similarities that favor the vector species, LACV infections are likely to occur in western Pennsylvania. It is possible that LACV is underrecognized and underdiagnosed in Pennsylvania, which may be due to a lack of awareness amongst healthcare providers. Moreover, the diagnostic procedure for LACV may be underutilized in detecting cases.
Improving awareness of LACV infections in western Pennsylvania is necessary. This article seeks to enhance awareness by defining its presence in Northeastern Ohio counties, especially in counties along the OH-PA border, and highlighting diagnostic pitfalls commonly encountered in confirming the infection. Improving awareness about LACV infections, especially among healthcare professionals, may positively impact the diagnosis of cases in the region, and thereby potentially improve patient management.
Author Bios
Diana Ortiz, Ph.D. Assistant Professor of Biology, Westminster College, PA
Dr. Ortiz has been studying vector borne diseases for over 20 years. She has authored and co-authored peer-reviewed articles in several journals and currently serves as an assistant professor of biology at Westminster College in New Wilmington, PA conducting undergraduate research in vector biology, disease ecology, and public health.
Zachary Fryda, B.S., former Clinical Research Assistant at Akron Children’s Hospital, OH
Zachary received a Bachelor of Science degree in Biology in May of 2019 from Westminster College, Pennsylvania. Zachary will be continuing his education at LECOM Lake Erie College of Osteopathic Medicine (LECOM)-Bradenton to pursue a degree in Doctor of Osteopathy.
John Bower, M.D., Pediatric Infectious Disease Specialist, Akron Children’s Hospital, OH
Dr. Bower is a Pediatric Infectious Disease Specialist at the Akron Children’s Hospital in Akron, Ohio.
Throughout the year, our writers feature fresh, in-depth, and relevant information for our audience of 40,000+ healthcare leaders and professionals. As a healthcare business publication, we cover and cherish our relationship with the entire health care industry including administrators, nurses, physicians, physical therapists, pharmacists, and more. We cover a broad spectrum from hospitals to medical offices to outpatient services to eye surgery centers to university settings. We focus on rehabilitation, nursing homes, home care, hospice as well as men’s health, women’s heath, and pediatrics.