The abdominal transplant team at Allegheny Health Network’s (AHN) Allegheny General Hospital (AGH), has joined a select group of medical centers around the country that perform living donor liver transplants, a highly sophisticated procedure that provides an additional life-saving option for some patients with end-stage liver disease.
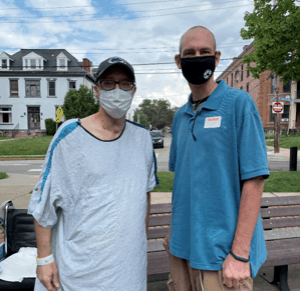
After nearly a nine-year battle with nonalcoholic fatty liver disease (NAFLD) the condition of James “Jim” Platzer, a 52-year-old man of Johnstown, PA, continued to worsen. The cirrhosis of his liver turned cancerous, and the severity of the illness put him on the national transplant waiting list. Only a few days after being listed, Platzer received a call that his friend, Matt Schraeder, with whom he volunteers with in the charity organization, 501st Legion, was a match and willing to be a living donor.
On June 28, 2021, Tadahiro Uemura, MD, PhD, system chief of the AHN Center for Abdominal Transplantation and surgical director of liver transplantation at AGH, removed 65% of the right lobe of Schraeder, a 41-year-old man from Morgantown, WV, through an abdominal incision. In an adjacent operating room, Ngoc Thai, MD, PhD, system director of the AHN Center for Abdominal Transplantation, successfully transplanted that liver into Platzer.

Living liver donation surgery requires comprehensive pre-transplant screening and planning protocols as well as precise coordination by the transplant team at the time of surgery. Surgeons begin by removing part of a person’s healthy liver – up to 65 percent – and using the partial liver to replace the recipient’s diseased liver. The procedures occur simultaneously. In the following few weeks, the livers of both the donor and recipient will regrow to the size of normal livers.
Livers are the second most-needed organ for transplant in the United States, after kidneys. Both chronic and acute medical conditions such as hepatitis C, alcoholic liver disease, infection, liver cancer or other genetic disorders, can cause the liver to stop working. Until a transplant becomes available, the only course of treatment for liver failure patients is medical maintenance of symptoms.
“While dialysis can bridge kidney failure patients until a transplant becomes available and cardiac assist devices can do the same for those with heart failure, there are currently no such bridge therapies or alternative treatments for end stage liver failure,” said Dr. Uemura. “That is why we are pleased to further advance our transplant program — by offering patients in need of a life-saving transplant the additional potential option of live donation.”
In the U.S., nearly 12,000 Americans are on the waitlist for a liver transplant yet only about 5,000 deceased-donor livers are available for transplant annually. Living-liver donation provides patients with an option that may expedite their access to a life-saving transplant much sooner than waiting for a deceased-donor liver match to become available.
“Due to the shortage of organ donors, about 10% of patients die each year waiting for a liver transplant. With the launch of our living liver transplant program, we are bringing another vital resource to our community and the patients we serve that will help lower the number of people with liver disease who suffer from lack of access to a donor organ,” said Dr. Thai.
Cirrhosis of the liver is an illness close to Schraeder’s heart, as he had considered being a living liver donor to his cousin before he passed of the disease. When Gina Platzer, the recipient’s wife, posted on social media asking for blood type O positive liver donors, Schraeder knew this was his chance to make a difference. The Platzers are incredibly moved by his selflessness with this donation.
According to the Organ Procurement and Transplantation Network, recipients of living donor livers have an average of 5 percent better long-term survival rate than deceased donor livers. Living donor liver transplant recipients also tend to recover sooner from the surgery, said Dr. Uemura.
In addition to the liver transplantation, AGH is a center for heart, kidney and pancreas transplants. In 2020, the hospital performed nearly 180 solid organ transplants, the highest in more than 30 years. AGH also has a partnership with Johns Hopkins Medicine for lung transplantation, providing western Pennsylvania residents with enhanced access to one of the country’s top programs. To learn more about AHN’s transplant program, visit AHN.org.
Throughout the year, our writers feature fresh, in-depth, and relevant information for our audience of 40,000+ healthcare leaders and professionals. As a healthcare business publication, we cover and cherish our relationship with the entire health care industry including administrators, nurses, physicians, physical therapists, pharmacists, and more. We cover a broad spectrum from hospitals to medical offices to outpatient services to eye surgery centers to university settings. We focus on rehabilitation, nursing homes, home care, hospice as well as men’s health, women’s heath, and pediatrics.