Understanding the Landscape of Musculoskeletal Pain
 Living with chronic pain can feel like an endless battle, especially when traditional solutions offer only temporary relief. Many of us have experienced the frustration of relying solely on medication, often with unwanted side effects.
Living with chronic pain can feel like an endless battle, especially when traditional solutions offer only temporary relief. Many of us have experienced the frustration of relying solely on medication, often with unwanted side effects.
Musculoskeletal pain is incredibly common, affecting nearly all of us at some point. It’s a widespread challenge that significantly impacts daily life and overall well-being. We’ve seen a growing shift in understanding how best to manage this pain, moving beyond a medication-only approach.

This comprehensive guide moves ‘Beyond Medication’ to explore modern, holistic approaches for finding lasting musculoskeletal pain relief. We will dig into understanding its root causes and diagnostic journeys. Our article will explore a diverse range of effective non-pharmacological therapies and self-care techniques.
Our goal is to empower you with knowledge. We aim to help you make informed decisions about managing your pain.
Musculoskeletal pain is a broad term encompassing discomfort in the bones, muscles, ligaments, tendons, and nerves that make up our body’s structural system. It’s the most common form of non-cancer pain, affecting virtually everyone at least once in their lives, often stemming from a simple muscle strain. However, chronic (long-term) musculoskeletal conditions, such as lower back pain, are also incredibly prevalent and can significantly impact daily life. In fact, low back pain stands out as the most common type of musculoskeletal pain globally.
The causes of musculoskeletal pain are as varied as the structures involved. Often, it’s the result of:
- Injury: This is the most common cause, ranging from acute trauma like falls, sports injuries, or car accidents, to fractures, sprains, and dislocations.
- Overuse and Repetitive Strain: Engaging in the same movements repeatedly, whether at work, during hobbies, or in sports, can lead to inflammation and damage in muscles, tendons, and joints.
- Poor Posture and Body Mechanics: Sustained incorrect posture, especially during prolonged sitting or standing, or using improper lifting techniques, can place undue stress on the spine and other joints, leading to pain.
- Underlying Health Conditions: Many systemic diseases can manifest as musculoskeletal pain. These include various forms of arthritis (like rheumatoid arthritis, osteoarthritis, psoriatic arthritis, and gout), fibromyalgia, osteoporosis, and connective tissue diseases such as lupus. Infections affecting bones, muscles, or soft tissues can also be a source of acute pain.
- Nerve Compression: Conditions like carpal tunnel syndrome, cubital tunnel syndrome, or tarsal tunnel syndrome, where nerves are compressed, can cause pain, tingling, and numbness. Pressure can arise from repetitive use, leaning on elbows, or even underlying conditions like arthritis.
- Referred Pain: Interestingly, pain can sometimes feel like it originates in the musculoskeletal system, even when it stems from another organ. This is called referred pain and can originate from organs such as the heart, lungs, kidneys, gallbladder, spleen, or pancreas.
With over 150 different musculoskeletal disorders identified, understanding the specific type and cause of pain is crucial for effective management.

The Different Types of Pain
Musculoskeletal pain isn’t a monolithic experience; it manifests in various forms depending on the affected tissue:
- Muscle Pain (Myalgia): This can range from a deep, steady ache to sharp, localized pains. Causes include injury, infection, cramps, spasms, or even conditions like fibromyalgia, which causes widespread pain in tendons, muscles, and joints.
- Bone Pain: Often described as dull and achy, bone pain can become sharper and more intense if there’s a fracture or injury. It can also stem from infections, osteoporosis, or, rarely, tumors.
- Joint Pain (Arthralgia): This pain can be constant or intermittent and is often accompanied by swelling, stiffness, and a limited range of motion. It can feel sore, achy, throbbing, burning, or grating, commonly associated with arthritis.
- Tendon & Ligament Pain: Tendons connect muscles to bones, while ligaments connect bones to other bones. Pain in these areas is frequently the result of sprains, strains, or inflammation (tendinitis/tenosynovitis), often caused by overuse or sudden, unnatural movements.
- Nerve Compression Pain: This occurs when nerves are pinched or pressured, leading to sharp, shooting pain, tingling, numbness, or weakness. Common examples include sciatica (pain radiating down the leg from the lower back) or conditions affecting nerves in the wrist (carpal tunnel) or elbow (cubital tunnel).
- Fibromyalgia: This chronic condition causes widespread pain throughout the body, often described as a constant dull ache, accompanied by fatigue, sleep problems, and tenderness in specific areas.
Common Symptoms to Recognize
While the experience of musculoskeletal pain is highly individual, several common symptoms can indicate its presence:
- Aching & Stiffness: A persistent, dull ache in muscles or joints, often worse after periods of inactivity or in the morning. Stiffness can limit movement and flexibility.
- Burning Sensations: A distinct burning feeling, particularly common with nerve-related pain or localized inflammation.
- Fatigue: Persistent pain can be physically and mentally draining, leading to generalized tiredness and reduced energy levels.
- Sleep Disturbances: Pain often interferes with the ability to fall asleep or stay asleep, creating a vicious cycle where lack of sleep can exacerbate pain.
- Muscle Twitches or Spasms: Involuntary muscle contractions can be a symptom of muscle strain, nerve irritation, or conditions like fibromyalgia.
- Decreased Range of Motion: Difficulty moving a joint or limb through its full, normal range, often due to pain, swelling, or stiffness.
- Swelling and Redness: Visible signs of inflammation around a joint or injury site.
- Weakness: A reduction in muscle strength, making daily tasks challenging.
Recognizing these symptoms is the first step toward seeking appropriate care and finding effective musculoskeletal pain relief.
The Diagnostic Journey: From Symptoms to Strategy
Understanding musculoskeletal pain begins with accurately identifying its nature and origin. This diagnostic journey is critical, distinguishing between different types of pain and laying the groundwork for effective treatment.
A key distinction in pain management is between acute and chronic pain. Acute pain typically starts suddenly, often with a clear cause like an injury, and is short-lived, resolving as the body heals. In contrast, chronic pain persists for more than three to six months, sometimes even after the initial injury has healed, and can be a condition in itself. Chronic musculoskeletal conditions are very common, making this distinction vital for guiding treatment approaches.
Healthcare professionals employ a systematic approach to diagnose musculoskeletal pain:
- Medical History: This involves a detailed discussion about your symptoms, including when they started, what makes them better or worse, previous injuries, lifestyle, and any other health conditions.
- Physical Examination: A thorough physical assessment helps identify the affected areas, assess range of motion, evaluate tenderness, and check for swelling, redness, or muscle weakness.
- Diagnostic Imaging: Depending on the suspected cause, imaging tests may be ordered:
- X-rays: Useful for visualizing bones and identifying fractures, dislocations, or signs of arthritis.
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues, including muscles, tendons, ligaments, and nerves, helping to detect tears, inflammation, or nerve compression.
- CT Scans (Computed Tomography): Offers cross-sectional images, valuable for assessing complex bone structures and certain soft tissue issues.
- Blood Tests: These can help identify inflammatory conditions (like rheumatoid arthritis), infections, or other systemic issues contributing to pain.
- Nerve Conduction Studies/EMG: If nerve involvement is suspected, these tests measure electrical activity in muscles and nerves to pinpoint nerve damage or compression.
The importance of an accurate diagnosis cannot be overstated. It allows for the development of truly effective plans for Personalized musculoskeletal relief, moving beyond generic pain management to target the specific underlying issues. This custom approach ensures that the chosen therapies are not only appropriate but also have the highest chance of success, ultimately improving quality of life.
A Spectrum of Non-Medication Therapies for Musculoskeletal Pain Relief
In our journey to find lasting musculoskeletal pain relief, we are increasingly recognizing the power of non-medication therapies. These approaches are not only effective but also align with recommendations from health organizations like the CDC, which emphasize nonpharmacologic and nonopioid therapies as being at least as effective as opioids for many common types of acute pain. For subacute and chronic pain, these non-pharmacologic options are often preferred, minimizing the risks associated with long-term medication use.

Rehabilitative measures form the cornerstone of this modern approach. They focus on restoring function, reducing pain, and preventing recurrence through active patient participation.
The Role of Physical Therapy and Movement
Movement is medicine, and physical therapy is often the most critical component of a non-medication pain management strategy. The adage “motion is lotion” highlights how regular, guided movement can lubricate joints, improve blood flow, and strengthen supporting structures.
- Therapeutic Exercise: Custom exercise programs are designed to address specific weaknesses, imbalances, and restrictions. This can include strengthening exercises for core stability, resistance training to build muscle, and balance exercises to improve coordination.
- Stretching: Regular stretching improves flexibility, increases range of motion, and reduces muscle tension, which can be a significant contributor to pain.
- Improved Mobility: By working on strength and flexibility, physical therapy helps restore normal movement patterns, reducing strain on painful areas.
- Specialized Techniques:The McKenzie Method: This diagnostic and treatment system focuses on mechanical low back and neck pain, teaching patients self-treatment strategies to centralize and abolish pain.
- Tai Chi and Yoga: These mind-body practices combine gentle movements, stretching, and meditation. They are excellent for improving balance, flexibility, strength, and reducing stress, making them particularly beneficial for individuals with chronic pain or limited mobility. The U.S. Preventive Services Task Force recommends that adults get at least 150 minutes of moderate aerobic physical activity per week, in addition to at least two strengthening activities, and practices like Tai Chi and Qigong are excellent ways to meet these guidelines, even for those with limited motion.
Hands-On and Advanced Modalities
Beyond active exercise, a variety of hands-on and advanced modalities offer targeted musculoskeletal pain relief:
- Massage Therapy: Therapeutic massage can help relax tense muscles, improve circulation, reduce inflammation, and break down adhesions in soft tissues. It’s often used for conditions like low back pain, fibromyalgia, and muscle spasms.
- Chiropractic Care and Spinal Manipulation: Chiropractors focus on the relationship between the spine and nervous system. Spinal manipulation, or adjustments, aims to restore proper joint movement and reduce nerve irritation, often providing significant relief for back pain, neck pain, and headaches.
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body. It’s believed to stimulate the body’s natural pain-relieving mechanisms and is increasingly used for various types of acute and chronic musculoskeletal pain.
- Advanced Therapeutic Options: For more persistent or complex cases, advanced modalities can provide significant relief. A comprehensive approach to musculoskeletal pain relief often includes options like Laser Therapy, which uses focused light to reduce inflammation and promote healing at a cellular level; Shockwave Therapy, which uses acoustic waves to stimulate tissue repair and reduce pain; or Electrical Stimulation (TENS), which uses low-voltage electrical currents to block pain signals. Other innovative treatments include TECAR Therapy for deep tissue healing, Vax-D Spinal Decompression for disc-related pain, Emfield Pro for pain and inflammation, and Soft Tissue Manual Therapy to address muscle and fascia restrictions. These diverse treatments, often integrated into a personalized plan for Dr. Sheps musculoskeletal pain relief, offer powerful avenues for recovery.
Ergonomics and Posture Correction
Our daily environments and habits play a significant role in musculoskeletal health. Poor ergonomics and posture are common culprits behind chronic pain.
- Workstation Setup: An ergonomically designed workstation can prevent strain on the neck, shoulders, back, and wrists. This includes proper chair height, monitor placement, keyboard and mouse positioning, and regular breaks.
- Proper Lifting Techniques: Lifting heavy objects incorrectly is a primary cause of back injuries. Learning to lift with the legs, keeping the back straight, and holding objects close to the body can prevent significant strain.
- Body Mechanics: Being mindful of how we move throughout the day – sitting, standing, walking, and performing tasks – can prevent repetitive strain and maintain spinal alignment.
- Preventing Repetitive Strain: Identifying and modifying repetitive movements in work or hobbies is crucial. This might involve using ergonomic tools, varying tasks, or incorporating micro-breaks with stretching.

By proactively addressing these factors, we can significantly reduce the risk of developing musculoskeletal pain and support our body’s natural healing processes.
Self-Care and Prevention: Taking an Active Role
Empowerment in managing musculoskeletal pain often begins with self-care and preventative measures. Our daily lifestyle choices profoundly impact our musculoskeletal health, making these strategies fundamental for long-term relief and well-being.
Lifestyle Choices and Preventive Measures
- Healthy Diet: A balanced diet rich in anti-inflammatory foods (fruits, vegetables, whole grains, lean proteins) can reduce systemic inflammation, which often exacerbates pain. Avoiding processed foods, excessive sugar, and unhealthy fats can also be beneficial.
- Maintaining a Healthy Weight: Excess body weight places additional stress on weight-bearing joints like the knees, hips, and spine, contributing to pain and accelerating degenerative conditions.
- Quitting Smoking: Smoking is known to increase inflammation throughout the body and can impair healing, making musculoskeletal pain worse and recovery slower.
- Quality Sleep: Adequate, restorative sleep is crucial for the body’s repair processes. Chronic pain often disrupts sleep, creating a vicious cycle; prioritizing sleep hygiene can significantly improve pain management.
- Regular Physical Activity: As discussed, consistent movement, stretching, and strengthening are vital. This not only prevents stiffness but also strengthens muscles that support joints and bones.
Home Remedies for Effective Musculoskeletal Pain Relief
For acute flare-ups or mild to moderate pain, several home remedies can provide effective relief:
- RICE Method (Rest, Ice, Compression, Elevation): This classic approach is best for acute injuries.
- Rest: Avoid activities that aggravate the pain.
- Ice: Apply ice packs for 10-20 minutes at a time during the first 48-72 hours to reduce swelling and inflammation.
- Compression: Use bandages to reduce swelling.
- Elevation: Keep the injured area raised above the heart to minimize swelling.
- Heat Therapy: After the initial acute phase (typically 2-3 days), or for chronic stiffness and muscle aches, heat therapy can be beneficial. Warm compresses, heating pads, or warm baths can increase blood flow, relax muscles, and ease stiffness. Alternating between ice and heat can also be effective.
- Over-the-Counter Topical Creams: Products containing ingredients like menthol, camphor, or capsaicin can provide localized pain relief. Capsaicin cream, derived from hot chili peppers, for example, can significantly reduce joint pain by depleting substance P, a chemical that transmits pain signals. Consistent use is key for long-term benefits.
- Stress Reduction Techniques: Chronic stress can heighten pain perception and contribute to muscle tension. Practices like mindfulness meditation, deep breathing exercises, yoga, or spending time in nature can help manage stress and, consequently, pain.
While over-the-counter anti-inflammatory drugs like ibuprofen can be effective for acute pain, long-term use can carry risks, including kidney and gastrointestinal damage. Therefore, exploring non-pharmacologic options first, or using medication judiciously under medical guidance, is generally preferred.
Complementary and Alternative Approaches
The landscape of pain management is increasingly embracing complementary and alternative therapies, with Americans spending over $30 billion annually on these products and practices. While some lack rigorous scientific backing, a growing body of research supports the effectiveness of several options for musculoskeletal pain relief.
Here’s a list of evidence-based supplements and therapies:
- Turmeric (Curcumin): This spice contains curcumin, a powerful anti-inflammatory compound. Studies suggest it can help decrease inflammation, similar to some NSAIDs. For optimal absorption, turmeric should be consumed with fatty oils and black pepper.
- Omega-3 Fatty Acids: Found abundantly in fish oil, these fatty acids are known for their anti-inflammatory properties. Many studies have evaluated the effectiveness and safety of omega-3 supplements for various inflammatory conditions, including rheumatoid arthritis, showing they can decrease joint swelling and tenderness.
- Glucosamine & Chondroitin: These are natural components of cartilage. Supplements containing them have been found to reduce pain caused by cartilage loss, particularly in osteoarthritis. Chondroitin often improves joint function, while glucosamine may improve stiffness.
- Boswellia (Indian Frankincense): Extracts from the Boswellia tree have been shown in several studies to improve pain and physical dysfunction associated with chronic inflammatory diseases like osteoarthritis. Its active compounds, boswellic acids, may interfere with cellular processes that cause inflammation.
- Cannabidiol (CBD) Oil: Research into CBD’s benefits for pain is ongoing and promising. Studies suggest CBD can activate the endocannabinoid system, which plays a role in regulating pain, mood, and inflammation. However, the FDA has not yet approved over-the-counter CBD products for pain, and close attention to ongoing research and safety reports is advised.
- Acupuncture and Massage: As mentioned earlier, these hands-on therapies are gaining wider acceptance as effective complementary treatments for various musculoskeletal conditions.
Integrating these approaches into a comprehensive strategy for Musculoskeletal pain management can offer a multifaceted path to relief. Always discuss any complementary therapies or supplements with your healthcare provider to ensure they are safe and appropriate for your specific condition and do not interact negatively with other medications. The National Center for Complementary and Integrative Health (NCCIH) is a valuable resource for research-based information on these therapies.
Frequently Asked Questions about Musculoskeletal Pain
We understand that living with musculoskeletal pain can bring many questions. Here, we address some of the most common concerns to help you better steer your condition.
What is the difference between acute and chronic pain?
This distinction is fundamental to understanding pain and its management:
- Acute Pain: This type of pain is typically sudden in onset and short-lived, usually lasting less than three to six months. It’s often a direct result of an injury, infection, or disease, and it resolves as the underlying cause heals. For example, the pain from a sprained ankle or a muscle strain is acute.
- Chronic Pain: In contrast, chronic pain persists for three to six months or longer, and can continue even after the initial injury or illness has healed. Chronic musculoskeletal conditions like low back pain or fibromyalgia are very common. This type of pain can be much more complex, involving changes in the nervous system that make it a condition in itself, rather than just a symptom. Treatment approaches for chronic pain often focus on long-term management, functional improvement, and quality of life, rather than just eliminating the pain entirely.
When should I see a doctor for my pain?
While many instances of musculoskeletal pain can be managed with self-care, there are clear indicators that professional medical help is needed:
- Severe Pain: If the pain is intense, debilitating, or interferes significantly with your daily activities.
- Pain That Doesn’t Improve: If your pain doesn’t show signs of improvement within a few weeks of self-care, or if it worsens.
- New or Worsening Symptoms: If you develop new symptoms such as fever, chills, a rash, unexplained weight loss, or if your pain spreads to other areas.
- Numbness, Tingling, or Weakness: These symptoms, especially if they radiate down a limb, could indicate nerve involvement and require prompt evaluation.
- Pain Following a Significant Injury: Any pain resulting from a fall, accident, or trauma should be assessed by a healthcare professional to rule out serious injury.
- Loss of Bowel or Bladder Control: This is a medical emergency, particularly if accompanied by back pain, and requires immediate medical attention.
- Pain That Wakes You from Sleep: This can sometimes be a red flag for more serious underlying conditions.
Always err on the side of caution and consult a healthcare provider if you are concerned about your pain or if it significantly impacts your quality of life.
What are the long-term risks of ignoring musculoskeletal pain?
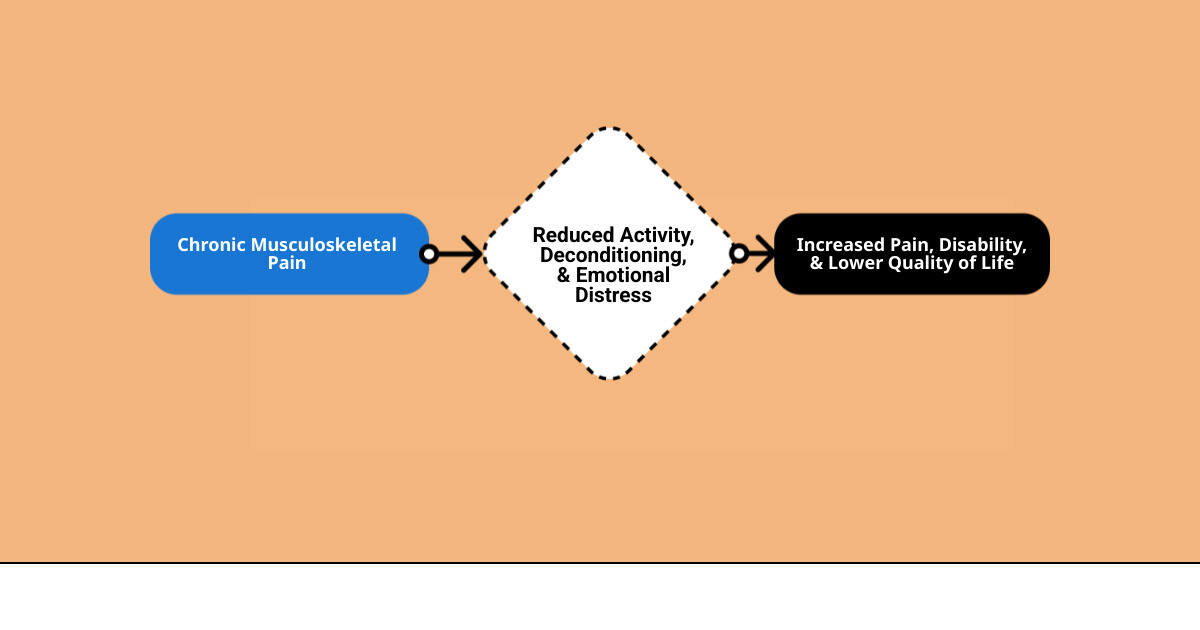
Ignoring persistent musculoskeletal pain can lead to a cascade of negative long-term implications that extend beyond just physical discomfort:
- Reduced Mobility and Function: Untreated pain can lead to guarding, muscle weakness, and joint stiffness, progressively limiting your ability to move and perform daily activities. This can result in a sedentary lifestyle, further weakening muscles and exacerbating pain.
- Chronic Pain Syndrome: Acute pain, if not properly managed, can sometimes transition into chronic pain, which is much harder to treat and can significantly impact overall well-being.
- Mental Health Challenges: Living with constant pain is emotionally taxing. It can lead to increased stress, anxiety, depression, irritability, and social isolation.
- Sleep Disruption: Chronic pain frequently interferes with sleep, leading to fatigue, reduced cognitive function, and a heightened perception of pain.
- Decreased Quality of Life: The cumulative effect of reduced mobility, mental health issues, and sleep problems can severely diminish your overall quality of life, affecting work, relationships, and leisure activities.
- Dependency on Medication: Delaying effective non-pharmacological treatments might lead to a greater reliance on pain medications, some of which carry risks of side effects or dependency.
- Structural Damage: In some cases, ignoring pain can allow underlying conditions, such as arthritis or disc degeneration, to worsen, potentially leading to more significant structural damage that might eventually require more invasive interventions.
Early intervention and a proactive approach to musculoskeletal pain relief are essential to prevent these long-term consequences and maintain a healthy, active life.
Conclusion
Navigating the complexities of musculoskeletal pain can be challenging, but the modern landscape of pain management offers a wealth of options beyond traditional medication. We’ve explored how a comprehensive understanding of your pain, coupled with a multi-faceted approach, can lead to lasting relief and improved quality of life.
From understanding the diverse types and causes of musculoskeletal pain to starting on a thorough diagnostic journey, we’ve seen that personalized care is paramount. The emphasis is increasingly on non-medication therapies – a spectrum of rehabilitative measures, physical therapy, hands-on modalities, and ergonomic adjustments that empower you to take an active role in your healing. Furthermore, integrating thoughtful self-care strategies and evidence-based complementary approaches can significantly improve your pain management plan.
The future of musculoskeletal pain relief is integrated and patient-centered, focusing on holistic well-being rather than just symptom suppression. By embracing these modern approaches, you can move beyond the limitations of medication-only solutions and find a path to sustained comfort and improved function.
While this guide provides valuable insights, your unique journey to musculoskeletal pain relief is best steered with professional guidance. We strongly encourage you to consult a healthcare professional. They can provide an accurate diagnosis, create a custom treatment plan custom to your specific needs, and help you integrate these strategies effectively into your life.
Throughout the year, our writers feature fresh, in-depth, and relevant information for our audience of 40,000+ healthcare leaders and professionals. As a healthcare business publication, we cover and cherish our relationship with the entire health care industry including administrators, nurses, physicians, physical therapists, pharmacists, and more. We cover a broad spectrum from hospitals to medical offices to outpatient services to eye surgery centers to university settings. We focus on rehabilitation, nursing homes, home care, hospice as well as men’s health, women’s heath, and pediatrics.
Disclaimer: The content on this site is for general informational purposes only and is not intended as medical, legal, or financial advice. No content published here should be construed as a substitute for professional advice, diagnosis, or treatment. Always consult with a qualified healthcare or legal professional regarding your specific needs.
See our full disclaimer for more details.